A 20 year old female came to casuality with chief complaints of fever since yesterday and altered sensorium since today morning
This is an online e log book to discuss our patient identified health data shared after taking his/her guardian signed informed consent. Here we discuss our individual patient problems through a series of inputs from available global online community of experts with a aim to solve those patients clinical problem with collective current best evidence based inputs.This blog also reflects my patient centered online learning portfolio and valuable inputs on the comments box is welcome.I have been given this case to solve in an attempts to understand the topic of patient clinical data analysis, to develop my competency in reading and comprehending clinical data including history, clinical finding, investigation.
PERSONAL HISTORY-
Diet- mixed
Appetite- normal
Sleep- adequate
Bowel and bladder movements- regular
No known allergies
Addictions- nil.
FAMILY HISTORY- not significant
GENERAL EXAMINATION-
patient is conscious, coherent, cooperative. Well oriented to time , place and person, moderately built and moderately nourished
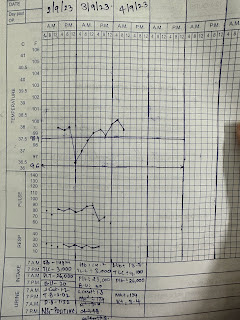
Vitals - at the time of presentation
BP- 150/100 mmHg
PR- 113 bpm
RR- 23 cpm
TEMP- 92 F
Spo2- 97%
*****GRBS- 540MG/DL AT THE TIME OF PRESENTATION.*****
NO SIGNS OF PALLOR, ICTERUS, CYANOSIS, CLUBBING, LYMPHADENOPATHY, OEDEMA.
SYSTEMIC EXAMINATION-
1) CVS- S1, S2 heard, no murmurs.
2) RS- BAE present, NVBS
3) PER ABDOMEN- soft , non tender, no organomegaly
4) CNS:
Higher mental functions - intact
Cranial nerves - intact
Motor examination - normal
Reflexes: R. L
Biceps. 2+ 2+
Triceps. 1+ 1+
Supinator 1+ 1+
Knee 2+ 2+
Ankle. 1+ 1+
Plantar. Flexor. Flexor
Sensory examination:Normal
No meningeal signs
INVESTIGATIONS-
30/9/23-
HEMOGRAM-
HB-11.1
TLC- 16700
MCV- 85.4
MCH- 26.5
MCHC- 31
PLT COUNT- 3.07
SERUM ELECTROLYTES-
Sodium- 136
Potassium- 4.2
Chloride- 109
SERUM OSMOLALITY- 287.8
RBS- 308
SERUM UREA- 30
SERUM CREATININE- 0.8
CUE-
Sugar++
Albumin +
Bile salts - nil
Bile pigments - nil
Pus cells- 3- 4
Epithelial cells- 2-3
LFT-
TB- 5.3
DB-1.22
AST-19
ALT-10
ALP- 240
TP- 7.1
ABG-
1/10/23 2/10/23
PH-7.13 7.42
PCO2 - 9.7 19.8
PO2 - 67.2 117
HCO3 - 3.1 12.8
ST. HCO3 - 7.3 16.9
BEB- 26.1 9.5
O2 SAT- 93.4 98.1
1/10/23-
SERUM ELECTROLYTES-
SODIUM- 133
POTASSIUM- 4.1
CHLORIDE- 104
PLBS- 263.
URINARY KETONE BODIES- POSITIVE
LDH- 579
COOMBS( direct and indirect) - negative
HBA1C- 7.0
ECG-









Comments
Post a Comment