A 55year old male came with yellow discolouration of eyes and fever
This is an online e log book to discuss our patient identified health data shared after taking his/her guardian signed informed consent. Here we discuss our individual patient problems through a series of inputs from available global online community of experts with a aim to solve those patients clinical problem with collective current best evidence based inputs.This blog also reflects my patient centered online learning portfolio and valuable inputs on the comments box is welcome.I have been given this case to solve in an attempts to understand the topic of patient clinical data analysis, to develop my competency in reading and comprehending clinical data including history, clinical finding, investigation.
A 55 year old male from valligonda , tile and granite fixer by occupation came to OPD
Chief complaints:- yellowish discolouration of eyes since 1 month.
HOPI :-
Patient was apparently asymptomatic 3 months back then he developed abdominal pain , sudden in onset, gradually progressive, intermittent , throbbing type pain , in the right hypochondrium region and epigastric region, it is non- radiating. There were no aggravating factors and was relieved on taking medication , which was given to him by a local pharmacist.( unknown medication)
2 months back he developed low grade fever, sudden in onset, continuous and associated with chills and rigour. It was relieved on taking medication. ( dolo )
One month back he developed yellowish discolouration of the eye, insidious in onset, gradually progressive and increased in intensity over past one week. He consumed ayurvedic medicine weekly once for one month but it didn’t give him relief.
( according to his mother she felt his eyes were yellow and she performed an old ritual which is followed in her village and confirmed that he might be having jaundice and brought him some ayurvedic medicine).
History of decreased appetite and weight loss since 1 month.
History of itching over the legs since 1 month , which was increased in the evenings and night.
No history of loose stools, clay coloured stools, nausea, vomiting, headache, dizziness, burning micturition, low urine output.
No history of haematemesis, malaena, constipation, abdominal distension.
No history of breathlessness, cough.
PAST HISTORY:-
-History of TB 35 years back where he took medication for 3 months only.
-Appendectomy 25 years back.
-RTA - 6 years back, where had a right knee fracture which was treated outside.
Not a know case of DM, HTN, asthma, epilepsy, CVA, CAD.
PERSONAL HISTORY:-
diet- mixed
Appetite is decreased
bowl and bladder movements- regular
Sleep- inadequate
Addictions- quarter alcohol daily from past 35 years and stopped taking alcohol from past 2 month
- consumes tobacco daily [ one pack per day ].
.
DAILY ROUTINE:-
Wakes up a 5am and extracts the milk from cows and distributes it.
At 7am, he freshens up and drinks tea
At 9am , eats breakfast ( rice with vegetable curry) and goes to work.
He works at construction site as tile and granite fixer.
At 2pm, he consumes his lunch ( again rice curry) and continues to work.
He returns home by 7pm and brings alcohol while coming back.
8 to 9pm , he drinks alcohol and eats dinner.
He stopped consuming alcohol from past 2 months.
Usually sleeps by 10 pm but is having trouble in sleeping for past 2 weeks.
FAMILY HISTORY:- not significant
ON EXAMINATION
GENERAL EXAMINATION:-
Patient is conscious, coherent and cooperative
Well oriented to time , place and person.
Moderately built and moderately nourished.
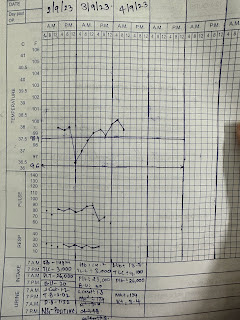
Vitals at presentation:
TEMP- 98.6 degrees Celsius
Pulse - 96 bpm regular normal volume
BP- 110/ 70 mmHg
RR- 18 cycles per minute.
Presence of icterus.
No pallor, clubbing, Cyanosis, lymphadenopathy, oedema.
SYSTEMIC EXAMINATION:
1) PER ABDOMEN:
INSPECTION:
-Shape of abdomen: flat
-Umbilicus: inverted
-Presence of appendectomy scar
-All quadrants are moving equally with respiration
-No engorged veins
- skin over the abdomen is smooth
-Hernial orifices intact
PALPATION:
-No local rise of temperature
- diffuse tenderness over the abdomen
-No Rebound tenderness
-No guarding rigidity
- liver not palpable
- spleen not palpable
Abdominal girth: 89 cm
PERCUSSION:
Shifting dullness - absent
No fluid thrill
Liver span - 9 cm
Liver dullness is not heard at 5th intercostal space.
AUSCULTATION:
On 12th Bowel sounds not heard
Today- diminished bowel sounds
2) CARDIOVASCULAR:
Inspection:
apex beat :5th ICS half inch medial to midclavicular line
Palpation:
inspectory findings confirmed, No thrills or parasternal heave
Auscultation: S1 , S2 heard and no murmurs
3) RESPIRATORY SYSTEM:
INSPECTION:
Shape of chest:Bilaterally symmetrical, Elliptical in shape
No visible chest deformities
No kyphoscoliosis,
Abdomino thoracic respiration, No irregular respiration
No tracheal shift
No dropping of shoulders, Spino scapular distance appears equal on both sides
no sinuses and scars
No engorged veins
PALPATION
Inspectory findings confirmed by Palpation
Chest movements - normal
Chest expansion-equal on both sides
PERCUSSION:
Resonant note heard over all areas
AUSCULTATION:
- coarse crepitations heard at right infra clavicular and right mammary areas.
- Norma vesicular breath sounds heard in all other areas.
-Vocal resonance: normal in all areas
4) CNS:
Higher mental functions :intact
Cranial nerves intact
Motor examination: R L
Bulk. N N
Tone. N N
Power. N N
Reflexes:
Biceps. 2+ 2+
Triceps. 2+ 2+
Supinator 2+. 2+
Knee 2+ 2+
Ankle. 2+. 2+
Sensory examination:Normal
No meningeal signs
PROVISIONAL DIAGNOSIS:-
DenovoHIV positive
Alcoholic liver disease?
Drug induced liver injury?
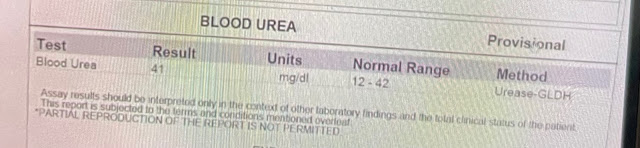
INVESTIGATIONS:-


















Comments
Post a Comment