A 60 year old male came with decreased vision since 2 years
This is an online e log book to discuss our patient identified health data shared after taking his/her guardian signed informed consent. Here we discuss our individual patient problems through a series of inputs from available global online community of experts with a aim to solve those patients clinical problem with collective current best evidence based inputs.This blog also reflects my patient centered online learning portfolio and valuable inputs on the comments box is welcome.I have been given this case to solve in an attempts to understand the topic of patient clinical data analysis, to develop my competency in reading and comprehending clinical data including history, clinical finding, investigation.
PERSONAL HISTORY-
Diet- mixed
Appetite- normal
Sleep- adequate
Bowel and bladder movements- regular
No known allergies
Addictions- chronic alcoholic since 20 years, consumes 90ml per day, preferred drinking brandy and whiskey , if not available he consumes toddy around 1 litre.
Chronic smoker since 20 years, consumes one pack of Beedi per day( 20 beedis per pack) but stopped 5 years back on doctors advice.
FAMILY HISTORY- not significant
GENERAL EXAMINATION-
patient is conscious, coherent, cooperative. Well oriented to time , place and person, moderately built and moderately nourished
Vitals -
BP- 130/80 mmHg
PR- 92 bpm
RR- 18 cpm
TEMP- 98.2 F
NO SIGNS OF PALLOR , ICTERUS, CYANOSIS, CLUBBING, LYMPHADENOPATHY, OEDEMA.
SYSTEMIC EXAMINATION-
1) CVS- S1, S2 heard, no murmurs.
2) RS- BAE present, NVBS
3) PER ABDOMEN- diffuse tenderness
no organomegaly
4) CNS:
Higher mental functions - intact
Cranial nerves - intact
Motor examination - normal
Sensory examination:Normal
No meningeal signs
PROVISIONAL DIAGNOSIS-
? Diabetic nephropathy ( peripheral) with right side Immature senile cataract.
K/C/O HTN since 2 years
K/C/O DM since 7 years.
INVESTIGATIONS-
Hemogram-
Hb- 11.1
PCV- 32.9
TLC- 8,900
RBC- 3.85
PLT count- 2.13
RBS- 244mg/dl
Blood urea- 51
Serum creatinine- 2.6
Sodium- 141
Potassium- 4.2
Chloride- 103
Total bilirubin- 0.66
Direct bilirubin- 0.16
ALT- 14
AST- 13
ALP- 320
Total proteins- 6.2
Albumin- 3.88
A/G ratio - 1.67
CUE -
Pus cells - 3-4
Serology- negative.
USG-5/1023
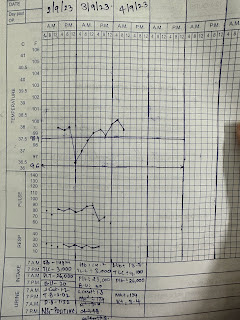
BP and GRBS charting-
6/10/23-
TREATMENT-
1. INJ. HUMAN ACTRAPID INSULIN SC / TID premeal
2. TAB. AMLODIPINE 5mg PO / OD 8am
3. TAB. PREGABALIN 75 mg PO/ HS 9pm
4.RE E/D CIPLOX QID
5. GRBS 7 PROFILE MONITORING
6. BP monitoring 2nd hourly.












Comments
Post a Comment