A 78 year old male came to casualty with weakness of right upper limb and lower limb since 4 days
This is an online e log book to discuss our patient identified health data shared after taking his/her guardian signed informed consent. Here we discuss our individual patient problems through a series of inputs from available global online community of experts with a aim to solve those patients clinical problem with collective current best evidence based inputs.This blog also reflects my patient centered online learning portfolio and valuable inputs on the comments box is welcome.I have been given this case to solve in an attempts to understand the topic of patient clinical data analysis, to develop my competency in reading and comprehending clinical data including history, clinical finding, investigation.
A 78 year old male came to casualty with
CHIEF COMPLAINTS -
c/o weakness of right upper limb and lower limb since 4 days.
C/o inability to talk since 4 days
HOPI-
patient was apparently asymptomatic 2 years back then he developed weakness of left upper limb and lower limb, sudden in onset, non- progressive, it was associated with slurring of speech, he went to a local hospital in Nalgonda and was treated conservatively , recovered within 5 days.
H/o weakness in the right upper limb and lower limb since 4 days, sudden in onset, non- progressive, no aggrevatin and relieving factors.
H/o inability to talk since 4 days, sudden in onset, non- progressive.
H/o hiccups since yesterday, continuous.
No H/o deviation of mouth.
No H/o involuntary movements, bowel and bladder incontinence
No H/o fever, burning micturition , vomiting
PAST HISTORY-
K/C/O CVA [ LEFT HEMIPARESIS ] 2 years back
K/C/O HTN since 2 years and is on tab. Amlong 5mg, tab. Atenolol 50 mg PO/OD.
NOT A K/C/O DM, epilepsy, asthma,TB, thyroid disorders.
PERSONAL HISTORY-
Diet- mixed
Appetite- decreased
Sleep- adequate
Bowel and bladder movements- regular
No allergies
Addictions- consumes alcohol or toddy occasionally
FAMILY HISTORY- not significant
GENERAL EXAMINATION-
patient is conscious, coherent, cooperative. Well oriented to time , place and person, moderately built and moderately nourished
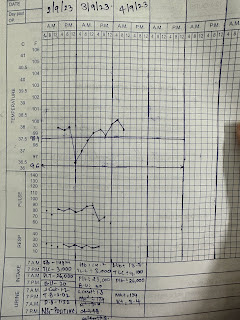
Vitals -
BP- 170/100 mmHg
PR- 80 bpm
RR- 16cpm
TEMP- 96.8 F
NO SIGNS OF PALLOR, ICTERUS, CYANOSIS, CLUBBING, LYMPHADENOPATHY, OEDEMA.
SYSTEMIC EXAMINATION-
1) CNS:
Higher mental functions - intact
Cranial nerves - intact
Motor examination: R L
Bulk. N N
Tone. UL Hypo Hypo
LL Hyper Hyper
Power. UL 0/5 3/5
LL. 0/5 2/5
Reflexes:
Biceps. 3+ 3+
Triceps. 3+ 2+
Supinator 2+ 2+
Knee 3+ 3+
Ankle. 3+ 2+
Plantar. Extensor. Extensor
Sensory examination:Normal
No meningeal signs
2) CVS- S1, S2 heard, no murmurs.
3) RS- BAE present, NVBS
4) PER ABDOMEN- soft , non tender, no organomegaly
PROVISIONAL DIAGNOSIS-
right hemiparesis with acute infarct in left superior frontal lobe ( left ACA territory )
With K/C/O left hemiparesis since 2 years.
K/C/O HTN since 2 years.
INVESTIGATIONS-
Hemogram-
On 9/9/23-
Hb - 13.4
TLC - 11000
Plt count- 3.18
PCV- 38.4
On 10/9/23
Hb- 13.3
TLC-14,300
Plt count- 3.1
PCV- 38.3
On 11/9/23
Hb- 13.4
TLC - 14,300
PCV- 39.6
Plt count- 3.21
9/9/23
Serum creatinine- 1.3
Serum Na+ 131
Serum K+ 3.2
Cl- 98
Blood urea- 41
RBS- 210
10/9/23
Urinary chloride- 189
Spot urinary K+ 25
Spot urinary Na+ 140
FBS - 259
CUE-






Comments
Post a Comment